Radiation-induced brain injury (RIBI) is a debilitating sequela after radiotherapy to treat head and neck cancer, with clinical manifestations including cognitive impairment and pathological changes such as brain tissue edema and necrosis. Although corticosteroids and bevacizumab can be used as first-line treatment at present, there are still a majority of RIBI patients fail to respond to or have contraindications to these two drugs. Therefore, there is an urgent need to develop new and better treatments for RIBI.
On Feb 22, 2023, Professor Yamei Tang's team from the Brain Research Center and Department of Neurology, Sun Yat-sen Memorial Hospital, Sun Yat-sen University published their work in Science Translational Medicine entitled "A phase II study of thalidomide for the treatment of radiation-induced blood-brain barrier injury". The work elucidates the mechanism by which thalidomide improves the blood-brain barrier and cerebral perfusion in radiation-induced brain injury through normalization of PDGFRβ in pericytes, providing new pathological insight and a potential therapeutic strategy for both brain diseases.
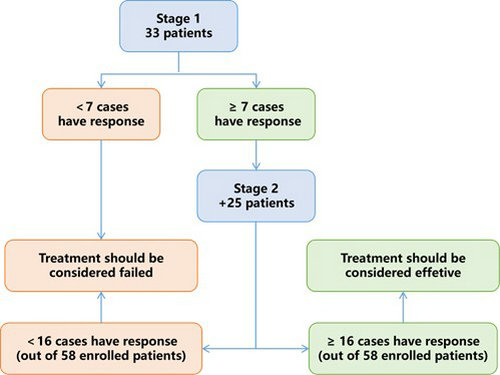
Potential therapatic effect of thalidomide on RIBI patients: A simon two stage design
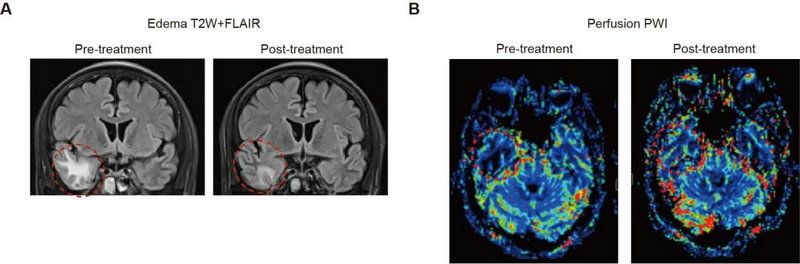
Thalidomide improves radiation-induced brain injury and cerebral perfusion
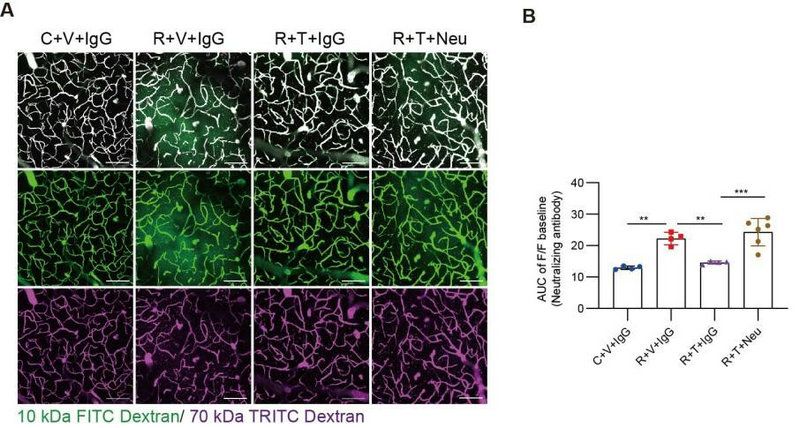
Thalidomide restores radiation-induced blood-brain barrier permeability by PDGFRβ
Thalidomide is a glutamate derivative, which was originally used as an antiemetic and sedative medication for pregnancy associated nausea and vomiting. The drug was later withdrawn because of its teratogenic effects. Recent studies have revealed the efficacy of thalidomide in treating gastrointestinal bleeding, hereditary hemorrhagic telangiectasia, and brain arteriovenous malformations by enhancing vascular integrity. Of note, human and animal studies have found that radiation-induced microvascular destruction plays a critical role in the pathogenesis of RIBI, but whether thalidomide could improve the cerebrovascular dysfunction after radiation injury has not yet been addressed.
Firstly, the author conducted a phase 2, single-arm, prospective trial to test the efficacy and safety of thalidomide in patients with RIBI who were resistant to or had contraindications to bevacizumab and corticosteroids. From the total of 58 patients enrolled, 27 (46.6%, 95%CI 33.3%-60.1%) met their primary outcome of the reduction of cerebral edema on MRI. Twenty-five (43.1%) patients demonstrated a clinical improvement based on the Late Effects Normal Tissues–Subjective, Objective, Management, Analytic (LENT/SOMA) scale, and 36 (62.1%) experienced cognitive improvement based on the Montreal Cognitive Assessment (MoCA) scores. No more that grade 3 adverse event was observed. These results indicated that thalidomide was effective and safe for the RIBI treatment.
Next, the authors investigated the mechanisms of how thalidomide work in the treatment of radiation-induced brain injury. Functional MRI unveiled that thalidomide treatment repaired the blood-brain barrier and restored blood supply in the radiation-injured brain region. Animal experiments have confirmed that radiation reduces the expression of PDGFRβ protein in pericyte, mediating the increase of blood-brain barrier permeability after radiation, and thalidomide can restore the integrity of blood-brain barrier and cerebrel blood flow by reversing the expression of PDGFRβ protein and alleviating the morphological changes of pericyte, thus protect neurons and improve cognitive function.
Overall, through the integration of clinical trial and basic research, our findings therefore demonstrated the promising therapeutic effects and mechanisms of thalidomide for treating cerebral small vessel injury and cognitive impairment resulted from radiotherapy, which providing a new therapeutic option and opportunity for patients with clinically refractory radiation brain injury.
Dr. Jinping Cheng, Jingru Jiang and Baixuan He, Associate Professor Wei-Jye Lin, Chief Physician Yi Li from the Brain Research Center and Department of Neurology, Sun Yat-sen Memorial Hospital, Sun Yat-sen University were the co-first authors of the paper. Professor Yamei Tang was the corresponding author. The study was mainly funded by grants from the National Natural Science Foundation of China.
Link to the paper: https://www.science.org/doi/10.1126/scitranslmed.abm6543