Source: Zhongshan Ophthalmic Center
Edited by: Zheng Longfei, Wang Dongmei
Recently, Professor Jin Yuan’s team from the Zhongshan Ophthalmology Center of Sun Yat-sen University and Professor Wang Yan’s team of the Ocean University of China published a Research article entitled "Developing a New Treatment for Superficial Fungal Infection Using Antifungal Collagen-HSAF Dressing". Wang Yan and Yuan Jin (the last corresponding author) are the corresponding authors of this paper, and postdoctoral fellows Zhong Jing (Zhongshan Ophthalmic Center, Sun Yat-sen University), Yan Xiayi (Ocean University of China), Zuo Xin (Zhongshan Ophthalmic Center, Sun Yat-sen University) and postdoctoral fellows Zhao Xuan (Zhongshan Ophthalmic Center, Sun Yat-sen University) are the co-first authors of the paper. The team of Professor Du Liangcheng of the University of Braska-Lincoln and the team of Professor Li Yaoyao of Shandong University participated in this work.
Infectious keratitis is one of the most common blinding eye diseases in developing countries, which fungal keratitis is the most common infectious type, but there is a lack of broad-spectrum and effective antifungal drugs. The research team found that marine-derived
Lysobacter enzymogenes YC36 can produce abundant secondary metabolites, inhibit the growth of a variety of fungi and bacteria, and can inhibit fungal activity by inhibiting the synthesis of sphingomyelin in the fungal bacterial wall. The research team extracted HSAF with a purity of 95.3% from
L. enzymogenes YC36 through macroporous resin adsorption, HPLC purification and other methods, which proved that the extracted HSAF has inhibitory effects on various pathogenic fungi including
Aspergillus fumigatus and
Candida krusei. It was found that the signal molecule indole can significantly increase the production of HSAF by 5 times through the two-component system QseC/QseB, which greatly provides the efficiency of directional expression and secretion of engineered bacteria.
Through self-assembled biofilm loading technology, HSAF was successfully fabricated into a collagen composite dosage form (Col-HSAF) with a dense lamellar structure to form a drug loading space. Cytotoxicity experiments have shown that Col-HSAF has good biocompatibility, HSAF can be slowly released from Col-HSAF for 2 weeks, and the peak time of corneal drugs in the pharmacokinetic animal model is 3 hours. Effective concentrations are maintained for approximately 1-2 weeks. In the fungal keratitis mouse model, the clinical score of the cornea in the Col-HSAF intervention group was significantly lower than that in the voriconazole treatment group. At the same time, fluorescence microscopy and two-photon microscopy were used to visualize the corneal hyphae, which confirmed that the fungal density was reduced significantly in the Col-HSAF treatment group. To further expand the antifungal application scenarios of Col-HSAF, the researchers established a skin infection model of Candida albicans. The results suggested that Col-HSAF has the therapeutic effects to reduce the amount of fungus in infected skin, to reduce the formation of subcutaneous granulation tissue and ameliorate inflammatory cell infiltration. The healing efficacy of infected wounds with Col-HSAF was significantly higher than in comparison the efficacy of clotrimazole ointment. This research provides a new choice of ocular surface and skin antifungal drugs for the clinic, And the drug translation Col-HASF will be carried out right away.
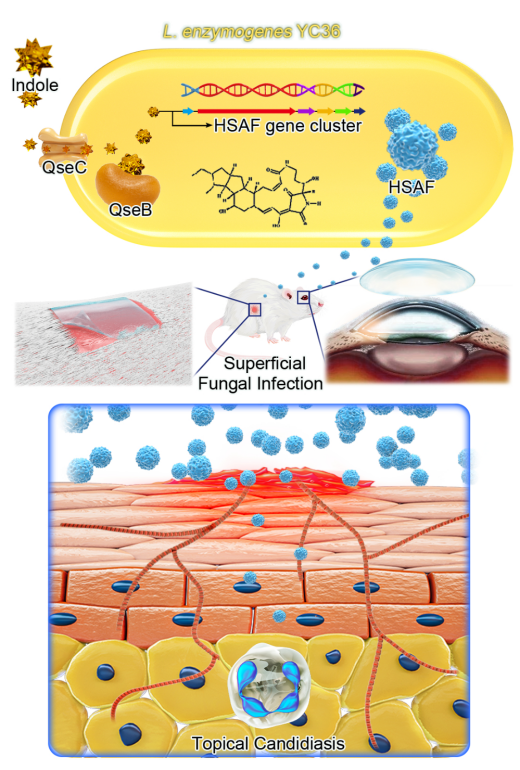
Schematic diagram of the mechanism of HSAF in the treatment of fungal keratitis and skin fungal infections
Link to the research article:
https://aiche.onlinelibrary.wiley.com/doi/epdf/10.1002/btm2.10304